
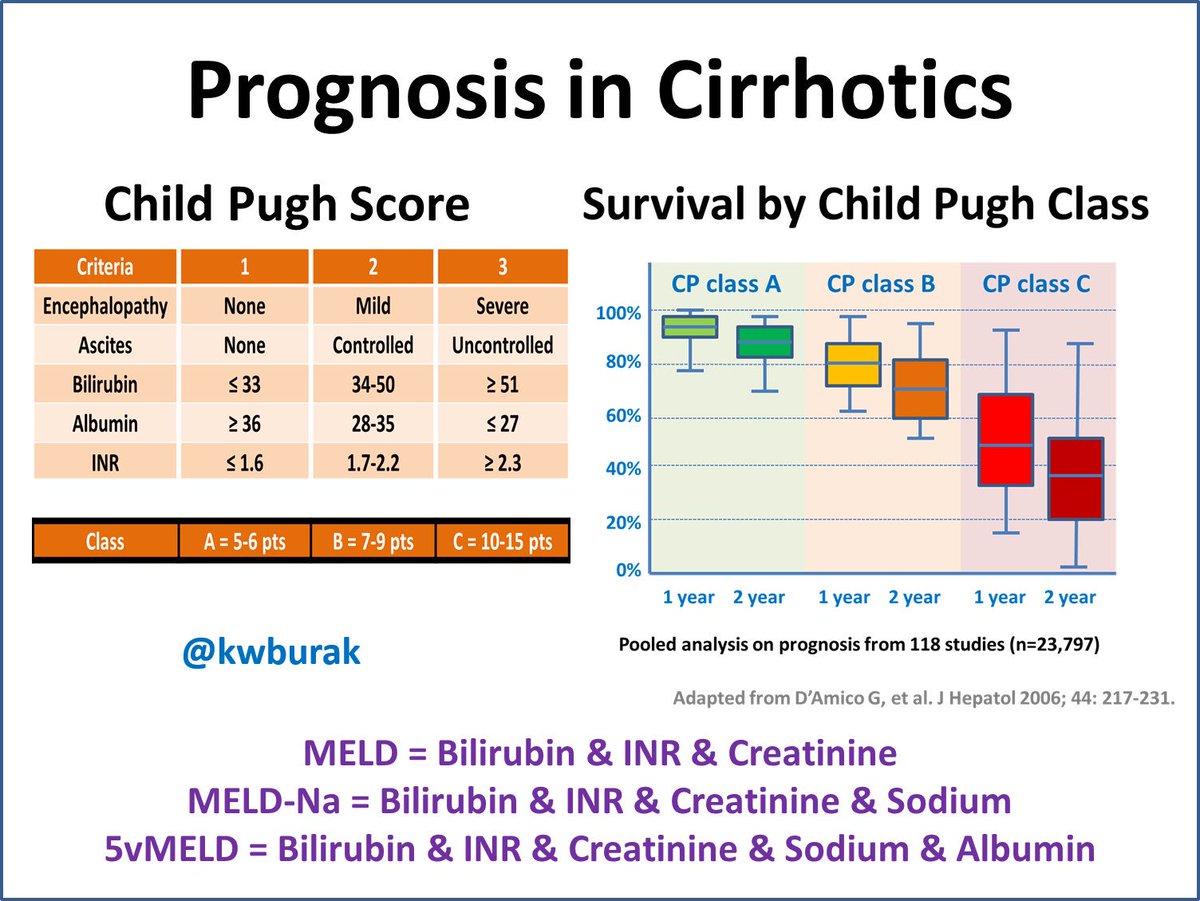
Nevertheless, it has some drawbacks such as subjectivity of clinical parameters and limited discriminant ability. The Child-Pugh score is still considered the cornerstone in the prognostic evaluation of cirrhotic patients although it was formulated more than 30 years ago. Over the years, many clinical and biochemical parameters have been suggested in order to more accurately predict the prognosis of cirrhotic patients and correctly assess their short and medium term survival. 3 Moreover, the economics, social burden, and ethical considerations of maintaining patients on waiting lists should also be taken into consideration. 2 Indeed, late transplantation affects patient outcome while performing OLT in those with less urgent indications penalises patients who could benefit most from the procedure. 1 The correct timing for surgery has an important impact on both mortality and morbidity of the patients.

There is an increasing discrepancy between the number of cirrhotic patients on waiting lists for orthotopic liver transplantation (OLT) and the number of available donor livers. TIPSS, transjugular intrahepatic portosystemic stent shunt.MELD, model for end stage liver disease.An increase in MELD score is associated with a decrease in residual liver function.
MELD SCORE 24 PROGNOSIS SERIES
MELD scores showed significant correlations with both MEGX values and Child-Pugh scores.Ĭonclusions: In a European series of cirrhotic patients the MELD score is an excellent predictor of both short and medium term survival, and performs at least as well as the Child-Pugh score. Serum creatinine, international normalised ratio, and MEGX 60 were independently associated with six month mortality while the same variables and the presence of ascites were associated with one year mortality. Child-Pugh and MELD scores, and MEGX serum levels were significantly different among patients who survived and those who died. Results: Thirty one patients died within the first year of follow up. MELD values were correlated with both Child-Pugh scores and MEGX test results. Multivariate analysis was performed on all variables to identify the parameters independently associated with one year and six month survival. The Child-Pugh score was calculated and the MELD score was computed according to the original formula for each patient.
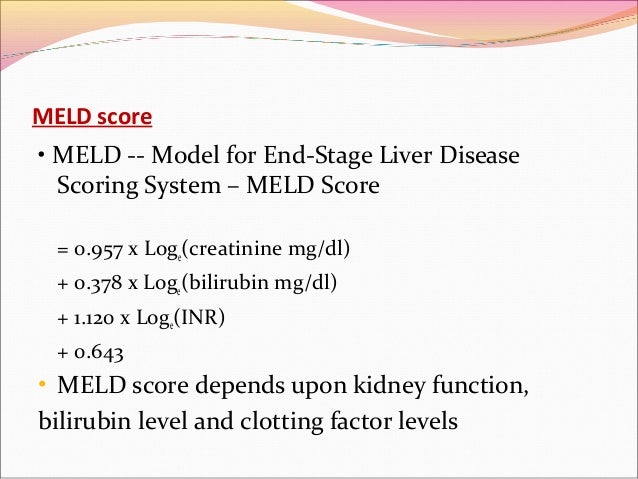
Patients and methods: We retrospectively evaluated survival of a cohort of 129 cirrhotic patients with a follow up period of at least one year. We also assessed correlations between the MELD scoring system and the degree of impairment of liver function, as evaluated by the monoethylglycinexylidide (MEGX) test. However, this model has not been validated beyond its original setting.Īim: To evaluate the short and medium term survival prognosis of a European series of cirrhotic patients by means of MELD compared with the Child-Pugh score. The model for end stage liver disease (MELD) has been proposed as a tool to predict mortality risk in cirrhotic patients. 4 A study including 140 patients undergoing TIPS showed that the MELD was more accurate than the CTP score for predicting three-month mortality.Background: Indices for predicting survival are essential for assessing prognosis and assigning priority for liver transplantation in patients with liver cirrhosis. The study showed: (1) the MELD, the CTP score, and the Emory score were similar in accuracy for predicting three-month mortality (2) the MELD was more accurate than the others for predicting 12-month mortality and (3) the MELD and the CTP score were more accurate than the Emory score for predicting 36-month mortality. The accuracy of each score was measured using the concordance-statistic (c-statistic): 1 was a score that perfectly predicted the outcome in question, and 0 was a score that failed to predict any outcome correctly. The mean age of patients was 57 years, about two thirds were men, and most had alcoholic cirrhosis. 4 The study used the version of the MELD that included creatinine, bilirubin, INR, and cause of cirrhosis. A German study compared the MELD, the CTP score, and the Emory score in predicting the prognosis of 162 patients with end-stage liver disease who were undergoing transjugular intrahepatic portosystemic shunting (TIPS).


 0 kommentar(er)
0 kommentar(er)
